Minimally Invasive Surgery
Minimally Invasive Spine Surgery (MISS) uses the latest advanced technology to treat back pain and neck pain caused by a variety of spinal conditions. Special surgical instruments, devices and advanced imaging techniques are used to visualize and perform the surgery through small incisions. The aim of MISS is to minimize damage to the muscles and surrounding structures enabling faster recovery and less pain.
Benefits of MISS
The benefits of MISS over the traditional open spine surgery include:
- Small surgery scars
- Less risk of infection
- Minimal blood loss during the surgery
- Minimal post-operative pain
- Quicker recovery
- Shortens the hospital stay
- Quicker return to work and normal activities
Some of the spinal conditions treated using MISS techniques are:
- Degenerative disc disease
- Spinal column tumors
- Infection
- Fractures
- Herniated discs
Procedure
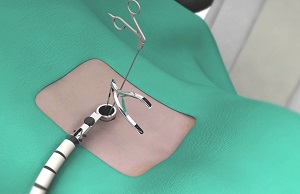
Minimally invasive spine surgery is performed through very small incisions. Through these small incisions, segmental tubular retractors and dilators are inserted to retract muscles away from the operative area and provide access to the affected area of the spine. This minimizes the damage to the muscles and soft tissues and lessens blood loss during the surgery. Surgical microscopes may also be used to magnify the visual field. Once the surgery is complete, the tissues fall back in place, as the various instruments are removed. The incision is then closed and covered with surgical tape.
Risk and complications
As with any surgical procedure, there are risks involved with minimally invasive spine surgery. The risks and complications of MISS may include infection, bleeding, nerve injury, or spinal cord injury as well as complications due to general anesthesia.
Extreme Lateral Interbody Fusion (XLIF)
- Degenerative disc disease: wearing out of intervertebral discs with age
- Scoliosis: abnormally curved spine
- Spinal stenosis: narrowing of the spinal canal
- Spondylolisthesis: slipping of vertebra from their normal position
- Fractures
- Infections and
- Tumour
- When the displacement of the vertebrae in degenerative spondylolisthesis is greater than 50%
- Severe compression of a spinal nerve
- Minimally invasive procedure which requires less surgical time reducing your time under anaesthesia.
- Less pain, scarring and blood loss as the procedure causes less damage to the adjacent tissues.
- Ensures early recovery and faster return to your normal activities.
- Formation of blood clots or deep vein thrombosis
- Improper fusion of the implant
- Injury to adjacent tissues
- Nerve or spinal cord damage
- Infection
- Pneumonia
- Urinary tract infection
- Stroke
The back is made up of a number of small bones called vertebrae. Cushioning discs present between the vertebrae act as shock absorbers. The vertebral column allows the cylindrical bundle of nerve fibres called the spinal cord to pass through the entire column length and branch out to the various parts of the body. Any damage or deformity to the bones of the vertebral column or to the intervertebral discs can damage these nerves, leading to pain in the body part that the nerve supplies.
Lateral lumbar interbody fusion also known as extreme lateral (XLIF) or direct lateral interbody fusion (DLIF) is a minimally invasive spinal procedure performed to treat back and leg pain caused by degenerative discs and other problems within the vertebral column. Interbody fusion involves the fusing of the affected vertebrae found in the lumbar region (lower back). In lateral lumbar interbody fusion, your doctor will access the spine from incisions made in your side.
Indications:
Lateral lumbar interbody fusion is indicated for:
Contraindications:
XLIF is not recommended in the following situations:
Surgical procedure:
When medication and conservative treatments fail to improve your back pain, your doctor may recommend a lateral lumbar interbody fusion procedure (XLIF).
XLIF usually takes about one hour and is performed under general anaesthesia. You will be placed on the operating table, positioned on your side. Your surgeon will use X-rays to identify the location of the degenerated disc and will mark your skin over this area of your spine. A small incision is made in your lower back region through which your surgeon inserts a finger to protect the abdominal lining from the instruments to be inserted laterally. Your surgeon will then make a second incision on your side in order to introduce the operating instruments. X-rays and nerve monitoring devices are used during the procedure to prevent damage to the adjacent tissues and nerves.
Your surgeon removes the degenerated intervertebral disc and prepares the disk space for fusion. A stabilizing disk implant is inserted into the empty disc space. The implant may be filled with bone graft, which will help in the fusion of the two vertebrae. The implant helps maintain proper disk height and provides good support to the operated spinal segment. In some cases your surgeon may secure the implant with plates or screws for additional support. Once the implant is in position, final X-rays are taken to confirm proper placement of the implant. At the end of the procedure, the small skin incisions are closed with stitches and bandaged.
Post-Operative Care:
Recovery from lateral lumbar interbody fusion procedure varies from patient to patient. Depending on your condition you may be able to return home the same day after the procedure, or may have to stay in the hospital for a few more days. You may notice an immediate improvement in your symptoms after the surgery or they symptoms may disappear gradually. You may experience some pain at the incision sites. This is quite normal; your doctor may prescribe pain medications to alleviate your discomfort. As there is less damage to the adjacent tissues, you may be able to get up and walk around the night after your surgery. Most patients are usually able to return to their normal activities within a few months after XLIF.
Advantages:
The advantages of XLIF include
Risks and complications:
As with any procedure, XLIF is associated with certain risks and complications including:
Anterior Lumbar Interbody Fusion (ALIF)
- Severe lumbar (low back) or leg pain that is unresponsive to non-surgical treatment.
- Degenerative disc disorder of lumbar spine (pain due to damaged disc)
- Spondylolisthesis (slippage of one vertebra on another)
- Scoliosis (S-shaped curve of spine)
- Fractures of spine
- Tumors
- Spinal instability
Anterior lumbar interbody fusion (ALIF) is a surgery performed to correct the spinal problems in the lower back. The surgery can be implemented either as an open surgery or minimally invasive technique.
Indications:
The common indications of ALIF are:
Surgical procedure:
The ALIF surgery is usually performed under general anesthesia. The patient is positioned supine lying on the back. The surgeon makes an incision in the abdomen and retracts the muscles and various structures to enhance the clarity and accessibility to the anterior aspect of the vertebrae. The surgical approach is from the front of the vertebral body in the low back region. Your surgeon removes whole or a part of the damaged disc between two adjacent vertebrae followed by fusion of the same with or without the use of bone grafts. External implant materials such as rods, screws, plates, and wires may be fixed to the treated vertebrae to deliver extra support and stability during the healing process. At the end of the procedure, the structures are re-approximated and the skin is closed with sutures.
The success of surgery depends on various factors such as age, spinal condition, overall health status, and activity level of the individual.
Recovery:
The recovery period after ALIF surgery depends on the body’s healing capacity. The post-surgical hospitalization includes the rehabilitation program. If required your surgeon may prescribe pain medications or a brace and follow-up physical therapy upon discharge.
The period of your rest or inactivity depends on a few factors such as the type of surgical procedure and the approach used to access your spine, the size of the incision and presence of any complications. Return to work or normal activity depends on the type of work or activity you plan to perform. Usually 3 to 6 weeks is the ideal time of healing. With the advanced and innovative techniques, it is now possible to achieve improved fusion rates, short hospital stay with an active and rapid recovery period.
Strictly adhere to the post-operative instructions suggested by your spine surgeon to promote healing and reduce the possibility of post-operative complications.
Risks or complications of ALIF surgery:
The complications of the ALIF surgery include infection, nerve damage, blood clots or blood loss or bowel and bladder problem and any problem associated with anesthesia. The underlying risk of spinal fusion surgery is failure of fusion of vertebral bone and bone graft which usually requires an additional surgery.
Talk to your spine surgeon if you have any concerns or queries regarding ALIF.
Transforaminal Lumbar Interbody Fusion (TLIF)
- Degenerative Disc Disease: Wearing out of the intervertebral discs with age
- Scoliosis: Abnormally curved spine
- Spinal Stenosis: Narrowing of the spinal canal
- Spondylolisthesis: Forward dislocation of one vertebra over the other
- Fractures
- Infections
- Tumors
- Formation of blood clots or deep vein thrombosis
- Improper fusion of the implant
- Injury to adjacent tissues
- Nerve or spinal cord damage
- Infection
Introduction
Our spine is made up of small bony segments called vertebrae. These vertebrae are categorized into cervical or neck vertebrae, thoracic (upper back) and lumbar (lower back). Cushioning discs present between each vertebrae act as shock absorbers. A cylindrical bundle of nerve fibers called the spinal cord passes through the entire vertebral column and branches out to the various parts of our body. Any damage or deformity to the bones of the vertebral column or to the disks present between the vertebrae can damage these nerves, leading to pain in the body part that the nerve supplies.
Transforaminal lumbar interbody fusion (TLIF) is a minimally invasive fusion of the vertebrae of the lumbar region (lower back). It is designed to provide stability to the spine and treat back and leg pain.
Indication
Transforaminal lumbar interbody fusion is indicated for:
Surgical procedure
Your surgeon may recommend a TLIF when conservative measures (rest, physical therapy, and medications) fail to relieve your back and leg pain.
TLIF usually takes about 3 to 6 hours depending on the number of spinal segments treated. It is performed under general anesthesia so you will be asleep throughout the procedure. You will be given preoperative antibiotics to prevent infection, and will be placed in the prone position (lying on your stomach).
X-ray is used to confirm the location of the diseased segment. Your surgeon will then create a couple small incisions on your back. Your back muscles are separated and held in place with tubular retractors in order to clearly expose the diseased part of your spine.
Your surgeon then removes the lamina (roof of the vertebrae) to allow better visualization of the nerve roots. Your surgeon will then trim or remove the facet joints providing more space to the nerve roots. The nerve roots are then protected and gently moved aside. The diseased disk material is then removed. A disk implant known as a spacer made of bone, carbon-fiber, titanium, or a polymer is then inserted into the empty disc space. The implant provides proper disk height and acts as a scaffold for the new bone to grow. Your surgeon will then place small screws or rods in the upper and lower vertebral bodies to provide stability during the healing process. X-rays are then taken to document the correct location of the spacer. The retractors are removed, releasing the muscles to their normal position. The tissue layers are closed with sutures, the incisions closed using stitches or surgical staples, and a sterile bandage is applied over the surgical site. In time, the bone graft will fuse to create a solid bone.
Post-Operative Care
Most patients are able to go home in 2 to 3 days after the TLIF procedure. Mild pain is normal, for which you will be prescribed pain medications. You will be advised to wear a brace for three months after your surgery to support you while standing and walking. Physical Therapy and Occupational Therapy will instruct you on how to get in and out of bed properly and walk independently. You should not bend or twist at your waist or lift more than 5 pounds for 4 to 6 weeks until your back muscles are stronger and your pain subsides after your procedure. You may shower immediately after your procedure, but necessary precautions need to be taken to keep your surgical wound clean and dry. You may return to light duties 2 to 3 weeks after your surgery depending on your pain level. Moderate level work and light recreational activities are allowed 3 months after your surgery.
Advantages
One of the major advantages of TLIF is that it causes relatively less damage to the spinal structures which helps maximize the stability of the fusion. As TLIF is a minimally invasive procedure, the operative time, hospital stay, pain, blood loss, and risk of nerve and muscle injuries are reduced.
Risks and complications
As with any procedure, TLIF is associated with certain risks and complications including: